Evidence-Based Rehab Treatment has become such a popular buzzword in the mental health and substance addiction treatment community that it is often thrown around without any explanation as to what it means.
While the name “evidence-based rehab treatment” provides a clue, the details often get lost or go unexplained to the general community who is actually looking for treatment.
With so many different types of addiction programs, it’s difficult for a person to find the best one for his or her needs, and even harder for others to find a suitable facility for someone they care about.
It’s estimated that only 10 percent of recovery facilities utilize evidence-based substance abuse treatment, even though it is considered highly successful.
What is Evidence-Based Rehab Treatment?
At its most basic level, evidence-based rehab treatment uses therapies and methods that have shown to be successful for addiction recovery according to research and scientific testing methodologies.
Evidence-Based Treatment (EBT), sometimes referred to as science-based treatment or evidence-based practices (EBP), originated in the medical field in the1980s, but didn’t gain popularity until the term became more widely used in the 1990s.
In the early 2000s, the development of treatment models based on evidence from scientific research expanded to many different fields, including mental health and substance addiction treatment.
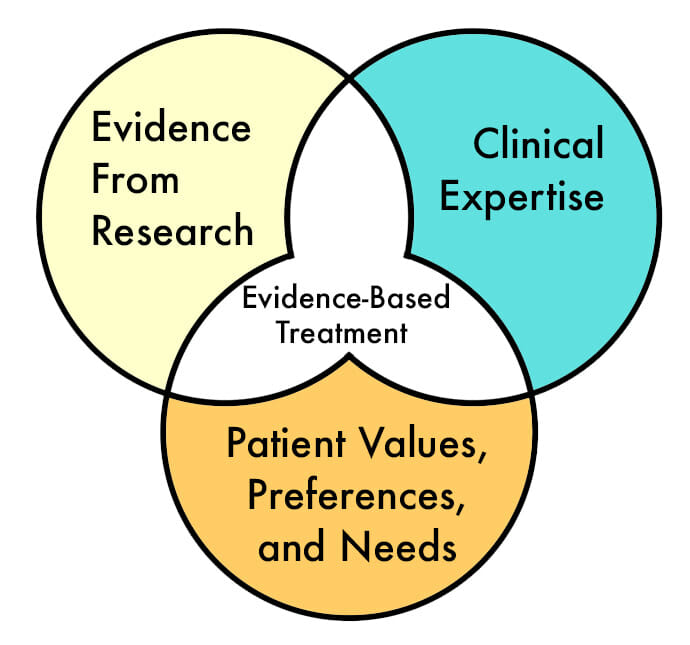
Evidence-based treatment practices integrate the following:
1. Evidence From Research
This involves using evidence-based treatment methods that are backed by research that has shown them to be helpful and effective for recovery.
2. Clinical Expertise
Patients are in the care of trained professionals who provide a proper clinical assessment and specialize in the treatment methods necessary for recovery.
3. Patient Values, Preferences, Needs, and Goals
Each patient’s individual needs and goals are considered with respect to treatment for their specific condition. This may relate to age, gender, environmental issues, readiness to change, and other personal factors that have an impact on his or her recovery.
The American Psychological Association states that evidence-based practices integrate “the best available research with clinical expertise in the context of patient characteristics, culture, and preferences.”
This decision-making process provides a framework for clinicians to determine the best possible treatment model for each patient’s recovery for his or her specific condition.
Evidence-based treatment practices involve conducting clinical assessments, referencing research, collaborating with the patient, and using treatment therapies that have proven to be successful for a particular condition.
Evidence-Based Treatment Therapies
Evidence-based treatment therapies are effective for addressing a wide range of disorders such as PTSD, anxiety, depression, drug or alcohol addiction, and co-occurring disorders of mental health and addiction together.
These therapies can be short-term interventions that run for a specified number of sessions or weeks, although many patients find the most success with a comprehensive program that lasts for 90 days or more for some conditions.
Treatment can be done with individuals, families, or groups, depending on the therapies needed and specific model of recovery.
Evidence-based rehab therapies can be provided in different settings, such as an outpatient clinic or a residential treatment facility.
Once mastered, a patient can continue to use the tools and techniques learned from these therapies at home after a formal treatment program has been completed.
Many treatment modalities can be used throughout the life span, while some need to be adapted for certain age groups.
Common evidence-based treatment therapies include:
- Cognitive Behavioral Therapy (CBT)
- Motivational Enhancement Therapy or Motivational Interviewing
- Relapse Prevention Therapy
- Contingency Management (CM)
- Dialectical Behavior Therapy (DBT)
- Medication Assisted Treatment (MAT)
- Rational Emotive Behavior Therapy (REBT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- 12 Step Facilitation Therapy
Most evidence-based treatment therapies require extensive training to properly implement specific interventions using different steps and tools. This allows practitioners to guide interventions in a consistent and systematic manner.
Medication Assisted Treatment uses evidence-based pharmacotherapies, which are medications that help withdrawal symptoms during detox, and others like Methadone or Suboxone to reduce cravings for opioids. There is much research to support the efficacy of these types of interventions.
Many of the other treatment therapies listed are evidence-based behavioral therapies that have proven through research and scientific studies to work well for alcohol treatment, drug addiction, PTSD, and related mental health conditions.
Cognitive Behavioral Therapy (CBT) is one of the most well known and widely used evidence-based rehab therapies for mental health and addiction recovery.
One of the main goals of CBT is to understand the relationship between our thoughts, emotions, and behaviors. By changing negative thoughts, we can improve our emotions and behaviors to more healthy patterns.
Relapse Prevention Therapy teaches techniques for recognizing triggers that might cause a person to begin using substances again, and ways to stay to remain abstinent.
Some of these therapies are specific to certain conditions, while others work for a range of conditions, and can be used to complement each other.
Components of Evidence-Based Rehab Models
While all recovery models will vary, there are core components that can be found in many. Because they are time-limited, the models are designed to equip patients with the necessary skills to manage their wellness over time.
Psychoeducation
Clinicians present information relevant to a patient’s health issues, which allows for insight into triggers, warning signs, and symptoms. The intent is for patients to gain self-awareness, identify their needs, and address any problem areas as they arise.
Skills Training
Patients learn how to manage their symptoms using appropriate coping mechanisms and distress-tolerance skills. They practice these skills on a consistent basis during calm periods in order to be better prepared in the presence of triggers.
Maintenance and Relapse Prevention
Once patients demonstrate a consistent alleviation of symptoms, they prepare for termination. Patients at this time should have the skills to independently manage their symptoms over time.
Goal of Evidence-Based Rehab Treatment
While evidence-based rehab methods are backed by research, not every treatment approach is going to work for everyone. There is no such thing as a one-size-fits-all treatment, but there are many options available, especially as more models emerge.
The ultimate goal of evidence-based rehab is to provide effective treatment methods that allow each patient to experience a lifelong recovery.
With that said, recovery may look different to each person depending on a number of factors. Relapse is a common component of addiction that affects some individuals and not others.
Even if a person does relapse, it should not be considered a failure. Recognizing it happened and getting back on track is an important part of recovery.
Evidence-based rehab aims to improve a person’s quality of life, physical and mental health, and personal relationships. It also strives to reduce risky behaviors that may lead to unwanted consequences.
There is a consensus among treatment providers about what works well based on research and past experience, with new methods being developed and tested all the time.
As evidence deems new approaches effective, they will no doubt be adopted for use as another successful recovery tool.