Table of Contents
It’s not surprising that many pharmacists and doctors now suggest non addictive painkillers and opioid alternatives for chronic pain management, instead of opiate prescription medications.
For the past few decades, doctors routinely prescribed opioid painkillers in large quantities for acute and chronic pain management, especially following an injury or surgery.
Even though they may have been appropriate in some cases, these highly addictive painkillers caused an epidemic of addiction and overdose.
Pain, whether caused by disease or injury, can be physically, psychologically, and emotionally debilitating.
While people suffering from acute pain often find relief as the body recovers from illness or physical trauma, the experience can still be troubling. For those suffering from chronic pain, the outlook can seem hopeless.
For these reasons, it makes sense that people in pain would be attracted to opioid painkillers. Not only were they readily available and overly prescribed, but they were also highly effective at treating short and long-term pain.
However, prescription opioid painkillers come with a serious downside because they are highly addictive.
For those who become addicted and try to stop taking them, the drugs can cause painful withdrawal symptoms.
Severe opioid withdrawal makes overcoming dependence and addiction extremely difficult and usually requires a drug detox program to safely manage the symptoms.
The Dangers of Opioids for Chronic Pain Management
The U.S. Department of Health and Human Services reports that in 2019, an estimated 9.7 million people misused or abused prescription painkillers.
While a small percentage of these people are recreational drug users, a vast majority of them are people with a prescription for drugs like Vicodin, Percocet, Hydrocodone, Oxycodone and others.
One of the primary reasons opioid painkillers should only be used for a short period of time is because a person quickly develops a tolerance to the medication. This means they need to take more of the drug to experience the same effects.
A person’s tolerance to opioids can develop in a relatively short amount of time, sometimes in just a few weeks. Most people think if a medication is prescribed, it is safe. That’s not necessarily true.
Those prescribed opioid painkillers can unknowingly develop a physical dependence to the drug by misusing it or taking it for longer than is necessary.
Even more alarming is the number of opioid related deaths in the past 20 years.
According to the Centers for Disease Control and Prevention, between 1999 and 2023, nearly 806,000 people died as a result of a fatal overdose to opioids. In 2023, nearly 105,000 died from a drug overdose and 76-percent of those involved an opioid.
Anyone who develops a dependency to these drugs should seek professional treatment for opioid, heroin, or fentanyl addiction.
Opioid use disorder is treatable, but severe hydrocodone or oxycodone withdrawal symptoms require most patients to be monitored by medical professionals during detox.
The addictive nature of prescription pain meds, along with the danger of fatal overdose, is why many in the healthcare industry are now only prescribing non-addictive painkillers.
Many doctors, pharmacists and pain specialists increasingly go to great lengths to provide opioid alternatives for chronic pain treatment.
List of Painkillers
Most pain medications have a brand name and a generic name that can be confusing.
It can also be difficult to know the difference between opioids and non-addictive painkillers when prescribed by a doctor. Below are some examples.
Opioids and Addictive Painkillers
- Oxycodone (OxyContin)
- Hydrocodone
- Oxymorphone
- Hydromorphone
- Morphine
- Codeine
- Tramadol (Ultram)
- Fentanyl (Duragesic)
- Heroin
Non Opioid Painkillers
- Ibuprofen (Advil and Motrin)
- Naproxen (Aleve)
- Acetylsalicylic Acid (Aspirin)
- Diclofenac (Voltaren)
- Ketorolac (Toradol)
- Fenoprofen (Nalfon)
- Suzetrigine (Journavx)
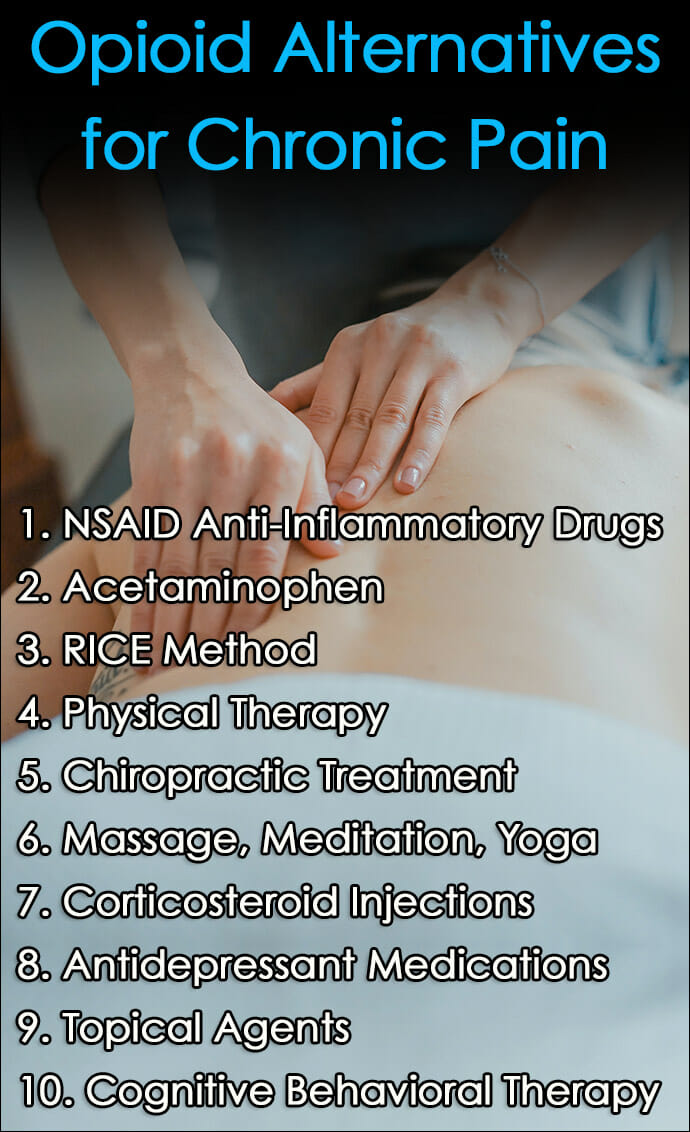
Opioid Alternatives for Chronic Pain Management
1. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Non-Steroidal Anti-Inflammatory Drugs, or NSAIDs, are over-the-counter pain medications like ibuprofen (Advil) and naproxen (Aleve).
NSAIDs are non-addictive painkillers that are not habit forming like opioids, and when taken as directed they reduce many forms of pain and inflammation.
2. Acetaminophen or Tylenol as Opioid Alternatives
Acetaminophen is generic for Tylenol and is another over-the-counter non-addictive painkiller. With Acetaminophen, it’s important to use it as directed and avoid alcohol because this combination can cause unhealthy side effects.
3. RICE Method
The RICE Method stands for Rest, ice, Compression and Elevation (RICE). This injury treatment approach can be effective at allowing the body to heal from pain and soft-tissue injuries, especially if started early and completed for the proper duration.
Rest gives the body time to heal the injury, while ice reduces swelling and pain. Compression supports the injured area and elevating it above the heart decreases inflammation and allows excess fluid to drain away from the injury.
4. Physical Therapy
Physical Therapy uses trained therapists who are knowledgeable about ways to help people strengthen and heal injured areas of the body.
Learning how to build strength and improve flexibility diminishes pain as well as reducing the likelihood of developing other injuries in the future.
5. Chiropractic Treatment
Chiropractic Treatment focuses on the body’s alignment to help reduce pain and improve function, primarily as it concerns the spine.
According to Harvard Health, modern chiropractors are also focusing on postural and exercise education, along with techniques for standing, walking, and sitting to limit unhealthy strain on the back.
6. Massage, Mindful Meditation, Yoga, and Exercise
While many people may tend to write-off approaches to pain treatment like Massage, Mindful Meditation, Yoga, and Exercise, there is plenty of evidence to suggest that they can have a serious impact on chronic pain.
For instance, mindful meditation has shown to quiet areas of the brain associated with pain.
Activities like massage can increase blood flow and reduce inflammation, while exercise and yoga movements strengthen the body and increase oxygen intake, which also promote healing.
All forms of movement have shown to be effective for improving physical and mental health by increasing endorphin production, which is the body’s own natural pain reliever.
It’s beneficial to know how to release endorphins through exercise and other activities because they are a natural alternative to opioids for pain.
7. Corticosteroid Injections
Corticosteroid Injections are powerful anti-inflammatories that are effective in reducing pain and inflammation in certain areas of the body, particularly the joints.
These pain management alternatives to opioids may be appropriate for some people to overcome pain, though this tends to be a short-term solution and people may experience varying lengths of relief.
Cortisone injections were once quite popular at reducing inflammation caused by injuries, but they are now only used for specific conditions.
8. Antidepressant Medication or Nerve Pain Prescriptions
In some instances, Antidepressant Medications or Nerve Pain Prescriptions serve as opioid alternatives to help reduce pain. These are often used as “off-label prescriptions,” meaning the medications are generally approved for something else other than pain.
The antidepressants Effexor (Venlafaxine) and Cymbalta (Duloxetine) are generally prescribed for depression, though both have shown to help ease pain associated with conditions like diabetic peripheral neuropathy, chronic bone or muscle pain, and fibromyalgia.
Gabapentin is a medication prescribed for epilepsy but is known to be effective in treating nerve pain brought on by illnesses like shingles and diabetes. It is also used for treating restless leg syndrome.
9. Topical Agents
Topical Agents or creams like Lidocaine and Capsaicin are rubbed directly on areas of the body experiencing pain, swelling, or both.
These topical agents have anti-inflammatory properties that can improve discomfort. They may also act faster than pills, which take time to enter the bloodstream.
10. Cognitive Behavioral Therapy for Chronic Pain Management
Cognitive Behavioral Therapy (CBT) is a skills-based treatment therapy that helps shift a person’s perception of pain and other issues by challenging engrained or negative thought patterns.
After a limited number of sessions with a counselor trained in CBT skills, people are often able to change the way they feel, even physically, by reframing their perception and thought processes related to a particular situation.
Additional Opioid Alternatives for Chronic Pain Management
The opioid alternatives for chronic pain management listed above are easy to incorporate and are generally accessible for most people.
Most of them have shown to be effective for many different types of pain and are much safer than opioids.
Other Alternatives to Opioid for Pain Include:
- Acupuncture
- Neurofeedback
- EPAT Therapy
- Biologics like PRP and Stem Cells
- Nerve blocks
- Epsom Salts and Magnesium
- TENs Units
- TMS Therapy
- Laser Therapy
- Marijuana
Some of these are less common than traditional treatments and may only work for certain types of pain or injuries. Nonetheless, quite a few people have found them to be quite effective.
Marijuana is a drug that isn’t legal in all states and is frowned upon as a treatment method by many people but has found a welcome community where medical cannabis is concerned.
It should be noted that it can be addictive and there are also known side effects of weed consumption. With that said, marijuana is much less dangerous or addictive than opioids.
When considering any method of chronic pain management, it is always highly recommended to consider non-opioid alternative painkillers first.
If opioids are necessary when non-addictive painkillers have not been successful, they should only be used sparingly for a short period of time, and only as prescribed.
FAQs About Opioid Alternatives
What are some strong painkillers that are not opioids?
Some NSAIDs, certain types of anticonvulsants or antidepressants, and several new prescription drugs are strong opioid alternative painkillers for severe pain.
Strong NSAIDs include Diclofenac (Voltaren) and Ketorolac (Toradol).
Suzetrigine (Journavx) is a new opioid alternative prescription pain medication recently approved by the FDA.
Why do people resort to opioid alternative pain meds?
The biggest reason for choosing opioid alternatives for chronic pain is to avoid the risk of dependence.
Opioids are highly addictive, but they also have other side effects that many people can’t tolerate, such as dizziness, constipation, and reduced mental focus.
Prescription opioids can be dangerous when used with other medications, and if a person develops a tolerance, they may stop being effective for providing pain relief.
What opioid alternative medication is similar to tramadol?
Suzetrigine (Journavx) is a new opioid alternative medication that is similar to tramadol for reducing moderate to severe pain.
Instead of attaching to opioid receptors in the brain like tramadol, it acts on the peripheral nervous system, which is a safer, non-addictive option for treating pain.
What is the safest pain medication for long term use?
It’s possible for any pain medication to carry some risk, especially if used for a long time or when not taken as directed.
Acetaminophen is one of the safest opioid alternatives for long-term use of chronic pain.
The biggest safety concern is the possibility of liver toxicity when taken with alcohol or in high doses, but it is generally safe when used properly.
It is always recommended to consult with a physician about the most appropriate medication for long-term, chronic pain.
How can I safely switch from opioids to opioid alternatives for chronic pain?
Do not discontinue prolonged opioid use all at once on your own. Long-term opioid use that causes a dependence may result in withdrawal symptoms if not managed properly.
The safest way to switch from opioids to opioid alternatives is to do so under the supervision of a doctor or detox specialist.
For those who are addicted to opioids, an addiction specialist may use medication assisted treatment therapies to safely transition to opioid alternatives over time. If you are unsure, it is recommended to seek help from a healthcare professional.